Task Group 113
Reference Organ and Effective Dose Coefficients for Common Diagnostic X-ray Imaging Examinations
Under Committee 2 and Committee 3
The primary dosimetric data on exposures in X-ray imaging procedures are measurements of entrance air kerma (for radiography), air kerma-area products (for diagnostic fluoroscopy), and CTDIvol and DLP (for computed tomography, CT). Such dose metrics are used to set Diagnostic Reference Levels that allow comparisons of doses received from the same procedure in different hospitals and help ensure that exposures are the minimum required to produce appropriate quality of images. However, effective dose is also used extensively in diagnostic x-ray imaging to provide a detriment-related dose quantity to inform clinical judgements, including the comparison of different x-ray procedures, and comparisons of imaging practice across different hospitals and medical facilities. For many years, the ICRP has produced, through its joint C2/C3 Task Group 36, reference dose coefficients for common diagnostic nuclear medicine procedures. However, ICRP has not provided reference dose coefficients for X-ray imaging procedures and consequently different methodologies are used to convert measurements to estimates of effective dose or some surrogate of effective dose. These calculations necessarily rely on disparate published data based on the use of older stylized hermaphrodite phantoms that are not in alignment with the most recent ICRP reference phantoms. In addition, different computational methods for radiation transport have been used to report organ doses from which the effective dose is computed. Those responsible for such calculations and their interpretation would welcome the availability of ICRP reference organ and effective dose coefficients.
Effective dose is also used to provide a common basis for assessing the medical component of radiation exposure to populations of individual countries or world-wide. Currently, the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) is assembling data on medical exposures in Member States. Meanwhile, the US National Council on Radiation Protection and Measurement (NCRP) is updating its Report 160, which is on medical exposures to the US population. The availability of ICRP reference dose coefficient for diagnostic X-ray procedures as well as nuclear medicine procedures would help standardize the reporting of doses for these applications.
The proposed Task Group has three major tasks. Task A is to define reference imaging exams for the ICRP reference individuals, male and female newborn, 1-year-old, 5-year-old, 10-year-old, 15-year-old, and adult, for radiography (both DR and CR), diagnostic fluoroscopy, interventional fluoroscopy, and computed tomography. These reference imaging exams would not be expected to cover the full range of clinical practice and would be limited to x-ray technique factors that would be clinically consistent with imaging the body morphometry of the reference individuals. For example, a reference abdominal CT exam would not encompass technique factors that would be needed for optimal imaging of a very short, and very obese adult male (e.g., kVp, mA, etc.) since the reference adult male is not short nor obese. These reference imaging exams would be developed within the Task Group with an eye toward consistency with national and international optimized and recommended imaging protocols for each modality. Reference imaging exams for interventional fluoroscopy would most likely be limited to common procedures that are anatomy focused (e.g., cardiac interventional procedures), fully acknowledging that each patient intervention can be highly variable regarding imaged anatomy, combination of fluoroscopy, cine, and radiographic spot imaging, and total procedure time. These reference imaging exams would be fully analogous to the reference biokinetic models established by Task Group 36 on diagnostic nuclear medicine organ and effective dose coefficients, recognizing that each individual patient may metabolize the radiopharmaceutical in a manner that may substantially differ from the reference model.
Task B is to perform Monte Carlo radiation transport simulations for the reference imaging exams and to report organ absorbed dose and effective dose coefficients for each of the reference computational phantoms and for each of the relevant reference imaging exam. The scope of this work would be limited to the use of the reference computational phantoms of the ICRP, male and female newborn, 1-year-old, 5-year-old, 10-year-old, 15-year-old, and adult. In addition, the Task Group would employ the recently developed ICRP pregnant female phantom series to include all, or a subset of, the 8-member phantom series: 8-week, 10-week, 15-week, 20-week, 25-week, 30-week, 35-week, and 38-week (post-conception) phantoms.
There are increasing demands by medical professions and relevant regulatory agencies to document patient-specific exposures to diagnostic medical imaging procedures. As such, various software tools have been developed which are built upon extensive libraries of computational phantoms covering a wide array of body morphometries, with algorithms for matching patient to phantom. Other methods, such as in CT, can even use the patient’s own CT image as the basis for a patient-specific phantom for dose assessment. These developments are beyond the mandate of the proposed task group. However, a Task C is proposed to compute and compare organ doses in the 10th and 90th body height / weight percentiles for patient populations with the values obtained for the reference individuals under Task B. When patient-specific organ doses (single gender) are weighted by radiation and tissue weighting factors, the result is not the effective dose (which is unfortunately widely reported), and this can be clarified in the report.
Progress of the various work strands of the Task Group can be summed up as follows:
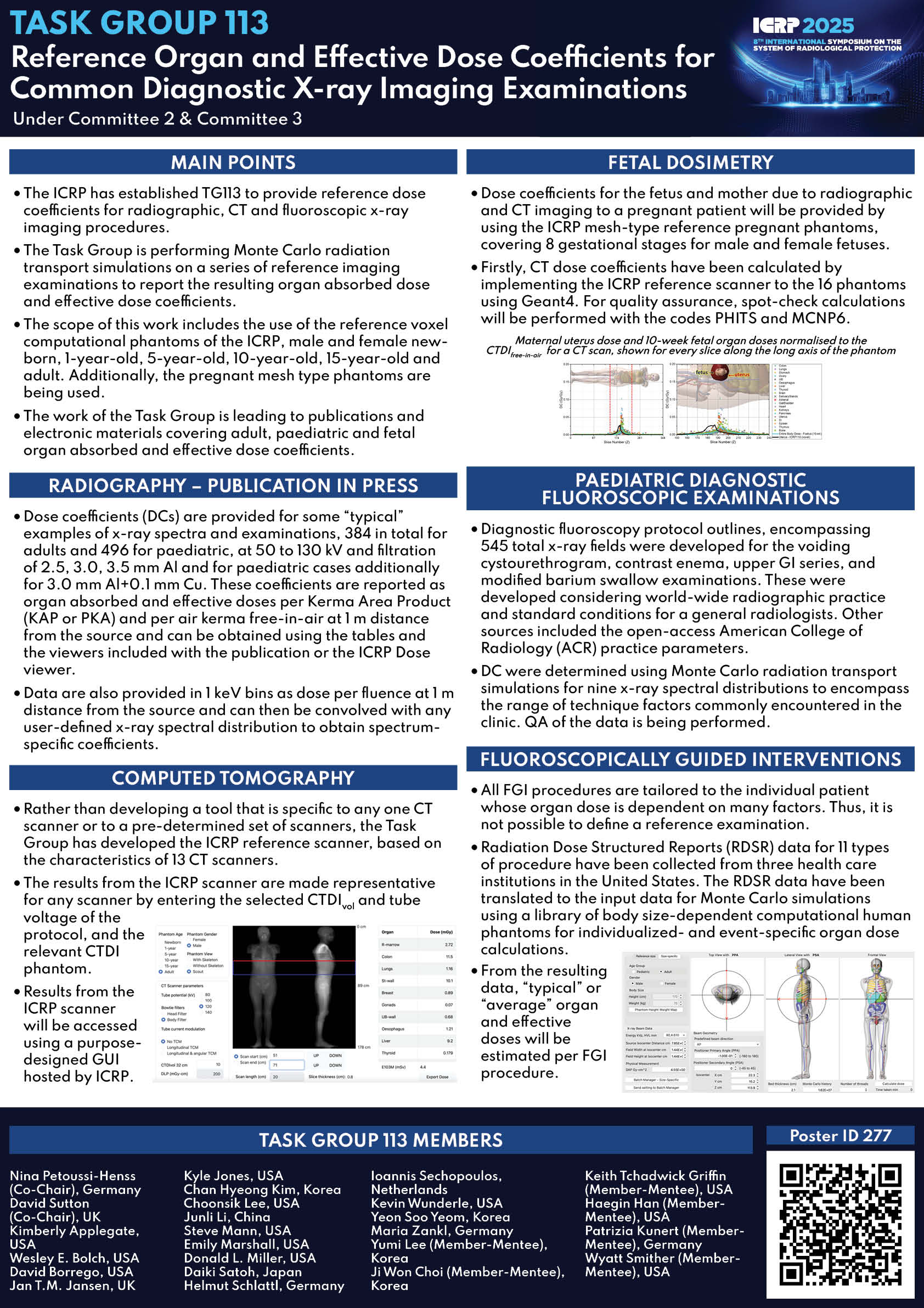
Radiography: Monte Carlo radiation transport simulations on the reference voxel computational phantoms of the ICRP male and female newborn, 1-year-old, 5-year-old, 10-year-old, 15-year-old, and adult have been performed for the most frequent radiographic examinations, considering good radiographic practice and standard conditions. Dose coefficients have been produced and the draft report will be open for public consultation in 2024. The ICRP Dose Viewer is being adapted to incorporate some of the resulting dose coefficients.
Computed Tomography: Rather than developing an approach to organ dosimetry that is specific to any CT scanner or a nominated set of scanners, the Task Group has developed a so-called ICRP representative scanner, based on the characteristics of 13 CT scanners from different manufacturers and 102 different operating conditions. The results from this scanner can be reliably matched to those of any other scanner using CTDI ratios. A Graphical User Interface to enable on the fly dosimetry has been developed and will be housed on the ICRP domain.
FGI: All FGI procedures are tailored to the individual patient whose organ dose is dependent on patient size, procedure complexity, and also operator, and equipment factors. There is a considerable range of the primary dosimetric quantity, Kerma Area Product (PKA ) and also mean PKA for every FGI procedure type. Thus, it is not possible to define a reference examination. The approach adopted assumes a “standard” examination and of a “reference” patient. Radiation Dose Structured reports (RDSR) data (10 types of FGI procedures, 100 patients per procedure) are in the process of being collected from three health care institutions in the United States. The RDSR data are being translated to the input data for Monte Carlo simulations combined with a library of body size-dependent computational human phantoms for individualized and event-specific organ dose calculations. From the resulting data, “typical” or “average” organ and effective doses will be estimated per FGI procedure. Work continues.
Paediatric Fluoroscopy: The Task Group have developed reference paediatric protocols for the voiding cystourethrogram, lower GI series, upper GI series, and modified barium swallow examinations carried out on paediatrics. Abnormal clinical diagnosis protocols have also been developed to address the most common or critical abnormal diagnosis. Monte Carlo calculations to determine organ and effective dose coefficients are ongoing.
Pregnant patients: work to commence May 2024.
ICRP 2025 Poster
| Nina Petoussi-Henss (Co-Chair), Federal Office for Radiation Protection (BfS), Germany | ||
| David Sutton (Co-Chair), University of Dundee, United Kingdom | ||
| Kimberly Applegate (Member), University of Kentucky COM (retired), USA | ||
| Wesley E. Bolch (Member), University of Florida, USA | ||
| David Borrego (Member), U.S. Environmental Protection Agency, USA | ||
| Jan T.M. Jansen (Member), United Kingdom Health Security Agency, United Kingdom | ||
| Kyle Jones (Member), The University of Texas MD Anderson Cancer Center, USA | ||
| Chan Hyeong Kim (Member), Hanyang University, Korea | ||
| Choonsik Lee (Member), National Cancer Institute, USA | ||
| Junli Li (Member), Tsinghua University, China | ||
| Steve Mann (Member), USA | ||
| Emily Marshall (Member), University of Florida Department of Radiology, USA | ||
| Donald L. Miller (Member), Center for Devices and Radiological Health Food and Drug Administration, USA | ||
| Daiki Satoh (Member), Japan Atomic Engergy Agency, Japan | ||
| Helmut Schlattl (Member), Bundesamt für Strahlenschutz, Germany | ||
| Ioannis Sechopoulos (Member), Radboud University Medical Center & Dutch Expert Centre for Screening (LRCB), Netherlands | ||
| Kevin Wunderle (Member), Cleveland Clinic, USA | ||
| Yeon Soo Yeom (Member), Yonsei University, Korea | ||
| Maria Zankl (Member), Germany | ||
| Yumi Lee (Member-Mentee), Yonsei University, Korea | ||
| Ji Won Choi (Member-Mentee), Yonsei University, Korea | ||
| Keith Tchadwick Griffin (Member-Mentee), National Cancer Institute, USA | ||
| Haegin Han (Member-Mentee), National Cancer Institute, USA | ||
| Patrizia Kunert (Member-Mentee), Federal Office for Radiation Protection (BfS), Germany | ||
| Wyatt Smither (Member-Mentee), University of Florida, USA | ||
| Chenxiao Wang (Technical Secretary), China Institute of Atomic Energy (CIAE), China |