Task Group 117
Radiological Protection in PET and PET/CT
Under Committee 3
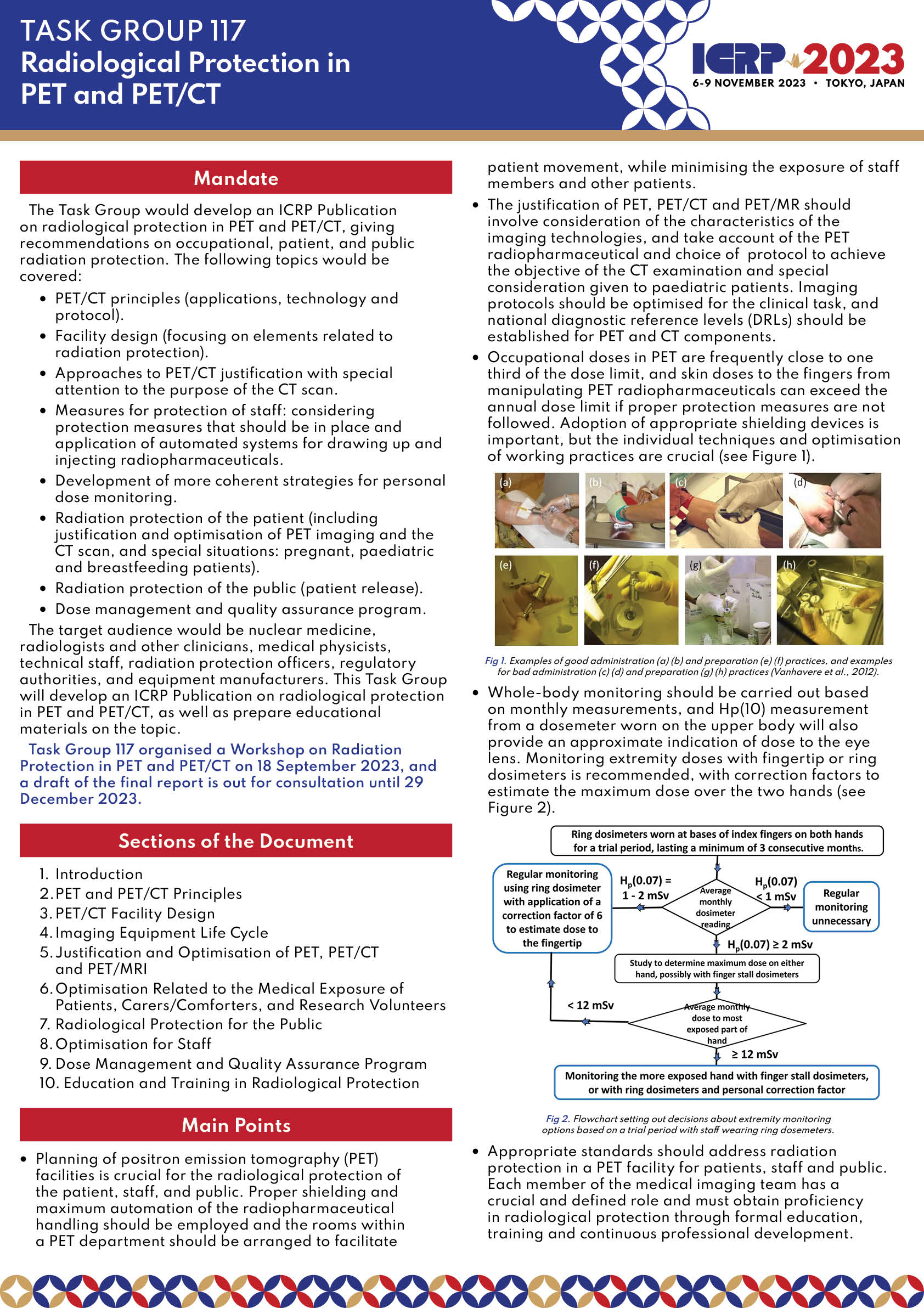
Positron emission tomography (PET) produces images of the distribution within the body of radioactive tracers that emit positrons. PET radiopharmaceuticals can be incorporated readily into biological molecules that have a growing role in oncology diagnosis, staging, treatment response and assessment for recurrence. PET is used together with computed tomography (CT) to provide better anatomical detail (hybrid fused images). Therefore, patients and staff are exposed to two different radiation sources. In some countries, PET/CT scans currently make up about 10% of all nuclear medicine examinations and about 20% of the effective dose delivered in nuclear medicine (European Commission, 2014). PET/CT imaging utilisation rates are growing as oncological, cardiac and neurological indications expand with the addition of new PET radiopharmaceuticals. The short half-lives of PET radionuclides and the high energies of annihilation -rays emitted (i.e. 511 keV) present particular challenges for staff radiation protection, which are compounded because patients are required to rest for an extended period between administration and imaging. While staff working in conventional Nuclear Medicine facilities typically receives annual effective doses of 0.1 mSv, occupational doses in PET are frequently close to 6 mSv. Skin doses to the fingers from manipulating PET radiopharmaceuticals can exceed the annual dose limit of 500 mSv if proper protection measures are not in place.
Large variations in staff doses are reported between centres which depend on the optimisation of facility shielding and design, the protection tools available, the techniques used by staff, and the level of experience and involvement of the staff in implementing protection methods. Approaches to monitoring finger doses and positions for wearing dosimeters proposed in the ORAMED project (7th EU Framework Programme, 2008-2011) differ from those recommended in Publication 106 (ICRP 2008). The recommendations were based on practices followed in different groups of centres and it is likely that, in addition to requirements for more optimisation of protection, dosimetry methods need to be tailored to local practices at each centre for realistic results to be obtained.
In relation to patient protection, radiation doses from PET/CT examinations depend not only on the administered activity, but also on the CT scan. The exposure factors should depend on whether the CT is simply to be used for anatomical localisation and attenuation correction, or to provide the necessary image quality for diagnosis with or without i.v. iodine contrast agent.
Public exposure is not a cause for concern, but some explanations are needed regarding the release of the patient after the PET scan.
The Task Group would develop an ICRP Publication on radiological protection in PET and PET/CT, giving recommendations on occupational, patient, and public radiation protection. The following topics would be covered:
- PET/CT principles (applications, technology and protocol)
- Facility design (focusing on elements related to radiation protection)
- Approaches to PET/CT justification with special attention to the purpose of the CT scan
- Measures for protection of staff: considering protection measures that should be in place and application of automated systems for drawing up and injecting radiopharmaceuticals
- Development of more coherent strategies for personal dose monitoring
- Radiation protection of the patient (including justification and optimisation of PET imaging and the CT scan, and special situations: pregnant, paediatric and breast-feeding patients)
- Radiation protection of the public (patient release)
- Dose management and quality assurance program
The target audience would be nuclear medicine, radiologists and other clinicians, medical physicists, technical staff, radiation protection officers, regulatory authorities, and equipment manufacturers. This Task Group will:
- Develop an ICRP Publication on radiological protection in PET and PET/CT
- Prepare educational materials on the topic
ICRP 2023 Poster
| Josep M Martí-Climent (Chair), Clínica Universidad de Navarra, Spain | ||
| Sandor Demeter (Member), University of Manitoba, Canada | ||
| Soeren Holm (Member), Denmark | ||
| Makoto Hosono (Member), Kindai University, Japan | ||
| Keon Kang (Member), Seoul National University, Korea | ||
| Mario Marengo (Member), University of Bologna, Italy | ||
| Colin Martin (Member), University of Glasgow, United Kingdom | ||
| Donna Newman (Member), USA | ||
| Ana Isabel Santos (Member), Hospital Garcia de Orta, E.P.E. - Almada, Portugal | ||
| Filip Vanhavere (Member), SCK-CEN, Belgian Nuclear Research Centre, Belgium |